Paying for Health Care: What’s Working Today, and What Does the Future Hold?
24 Jun 2014
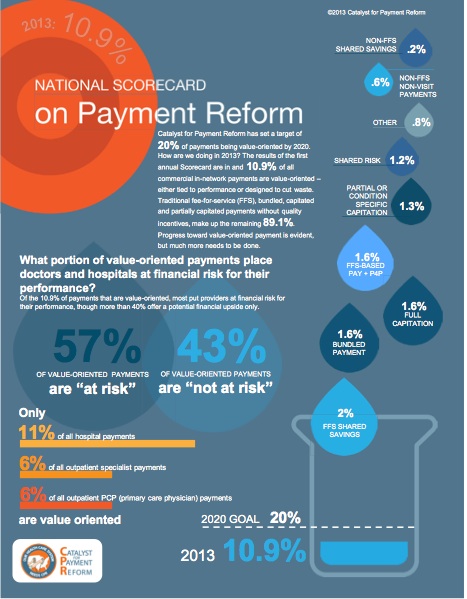
Health care payment reform is critical to employers and other health care purchasers looking to contain health care costs and get greater value for their spending. The current fee-for-service model can encourage unnecessary care, driving up costs as we pay for the volume of care instead of its value. Reforms aimed at the payment side of health care can cut waste and improve quality by changing providers’ incentive structure. At the same time, we need to focus on aligning incentives across consumers, health care providers, health care payers, and health care purchasers, which often requires pairing payment reforms with benefit and network designs that give consumers motivation to seek higher-value care.
 This report begins by defining payment reform, its penetration in the United States today, some of the current challenges, and the need to understand each specific market before determining an effective strategy for payment reform. The report then catalogues the payment, benefit, and network design reforms employers and others payers—including Medicare and states—are trying and how these strategies interconnect.
This report begins by defining payment reform, its penetration in the United States today, some of the current challenges, and the need to understand each specific market before determining an effective strategy for payment reform. The report then catalogues the payment, benefit, and network design reforms employers and others payers—including Medicare and states—are trying and how these strategies interconnect.
As health care costs continue to rise without a commensurate improvement in the quality of care, the major purchasers of health care, including employers, health plans, and state and federal government, are looking for ways to get better value for every health dollar they spend. There is tremendous variation in the approaches they pursue. Local market dynamics impact the reforms most likely to succeed. In charting a path forward, purchasers must consider a range of payment reforms, benefit and network designs, and how those designs can work together. Given how little we still know about what works, experimentation and rigorous evaluation are critical, as well as sharing lessons as we learn them.
You can find the full report by Catalyst for Payment Reform here.
