Background
Aligning Forces for Quality stipulates payment reform as one component of the Alliances’ improvement goals. Value-enhancing payment methods are necessary for high-value care, and successful payment reform methods reward, promote, and sustain improvement.[1] Two of the Alliances’ goals were to increase value (improved quality and lower cost) through outcome-focused payment reform and focus on reducing health care costs and spending in order to promote high-value health care.
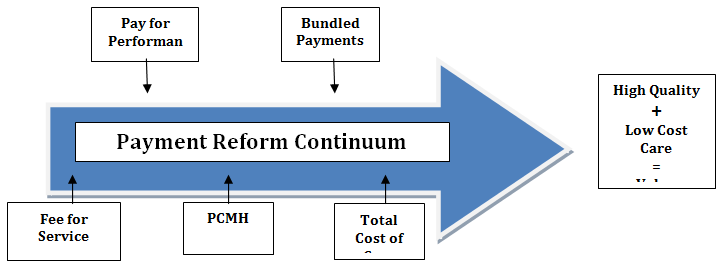
Payment reform in the context of AF4Q is distinct from other efforts because of the program’s geographic range. Traditional payment reform occurs within one setting—in a health system, for example—rather than across a community. This defining feature of AF4Q payment reform work has resulted in both challenges and success stories. Alliances are developing best-in-class information about the quality and cost of care and are working to make this information widely available to support health care decisions. As part of this effort, the Alliances are exploring new payment methods and convening stakeholders to build market support for such payment reform initiatives.[2] Alliances are developing and implementing a number of different payment reform models, including but not limited to shared savings, bundled payments, and medical homes. Figure 1 illustrates the continuum of payment reform strategies—there is a range in the accountability, risk tolerance, required integration, provider collaboration, complexity, and high-value care inherent within each of these approaches to payment reform.[3]
State of Payment Reform
Payment methods within the U.S. health care system are in urgent need of restructuring. Current payment methods, such as fee-for-service, exacerbate deficiencies among quality and cost of care. Current payment methods incentivize providers based on the volume of services delivered rather than on the quality of care,[4],[5] which ultimately leads to inflation of health care costs without corresponding improvement in outcomes. Certain initiatives within the Affordable Care Act (ACA) aim to address payment reform. For example, Medicare payments must be linked to quality outcomes, rather than just quality reporting.[6] The ACA also created the Center for Medicare and Medicaid Innovation “to test innovative payment and service delivery models to reduce program expenditures…while preserving or enhancing the quality of care.”[7]
Figure 1. Payment Reform Continuum[8]
[1] Aligning Forces for Quality Special Solicitation 2010 Call for Proposals.
[2] Ibid.
[3] CPR Payment Reform Framework, Catalyst for Payment Reform. http://www.catalyzepaymentreform.org/images/documents/CPR_Framework_053111.pdf.
[4] Margolius, D., and T. Bodenheimer. 2010. “Transforming Primary Care: From Past Practice to the Practice of the Future.” Health Affairs 29(5):779-784.
[5] Landon, B., J. Gill, R. Antonelli, and E. Rich. 2010. “Prospects For Rebuilding Primary Care Using The Patient-Centered Medical Home.” Health Affairs 29(5):827-834.
[6] Payment Reform. Health Services Research. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3029842/
[7] Centers for Medicare & Medicaid Services. http://innovation.cms.gov/about/index.html
[8] Joining Forces to Improve Health Outcomes in Metro Atlanta, Atlanta Regional Collaborative for Health Improvement. November 2013. http://www.archicollaborative.org/archi_playbook.pdf.