Improving Care Through Screening and Public Reporting
Colorectal cancer is the second leading cause of cancer-related deaths in the United States and the leading cause of cancer deaths among nonsmokers, according to the CDC. If everyone age 50 years and older had a regular screening test, at least 60 percent of the deaths from this cancer could be avoided. And early detection, the key to treating colorectal cancer, is inexpensive. Two communities in the Robert Wood Johnson’s Aligning Forces for Quality (AF4Q) initiative have made tackling this issue a priority.
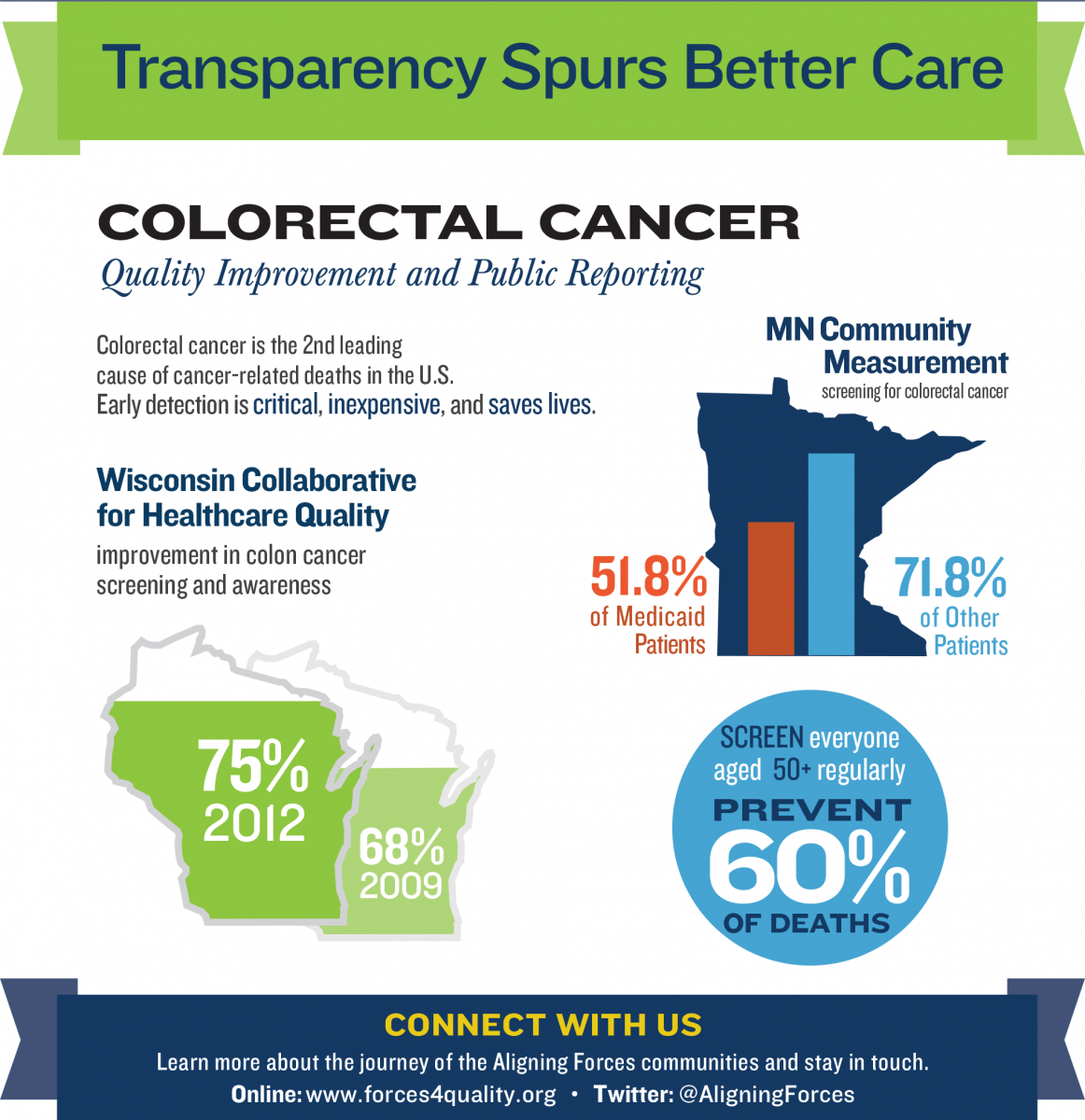
The Wisconsin Collaborative for Healthcare Quality (WCHQ), leader of the AF4Q initiative in Wisconsin, has improved its screening rates from 68 percent in 2009 to 75 percent in 2012. In 2012, more than half a million Wisconsinites received their preventive screening. To ensure continuing gains, WCHQ has established performance target goals for each of its 21 reporting member organizations. The ultimate goal is a 70 percent or higher screening rate for all patients.
WCHQ spurred change by engaging clinician leaders to identify best practices. A project team, including a dozen physicians and nurses, worked together over six months to select a set of proven best practices that include identifying eligible patients, redesigning clinic workflows, leveraging electronic medical records, improving patient-physician communications, and educating patients on different screening options. The proven best practices were presented through a series of webinars led by two physicians from the colorectal cancer project team.
Minnesota Community Measurement (MNCM) found that almost half of low-income adults in their state weren’t screened for colorectal cancer in 2013.
The disparity in screening rates is stark. Only 51.8 percent of Medicaid-covered adults ages 50 to 75 were screened for colorectal cancer in 2013, compared to 71.8 percent of those covered by other types of insurance.
Publicly reporting this information helps shine a light on this issue so providers and care systems recognize the gaps and take steps to close them.
“We’re focused on showing where medical groups have improved results for these patients and using that information to encourage other groups to make progress as well,” said MNCM President Jim Chase.
Read More:
- Wisconsin Partners with Consumer Reports to Publish Health Care Ratings
- Payment Reform Pioneers Deliver on Value
- Quality Field Notes: Data Reporting
- Medicaid Patient Received Fewer Colon, Cervical Cancer Screenings in 2013
